Human Papillomavirus (HPV) is a group of more than 100 related viruses that affect different parts of the body. About 40 of these can infect the genital area. HPV is mainly transmitted through skin-to-skin sexual contact. HPV may also be transmitted during genital-to-genital contact without penetration and oral sex.
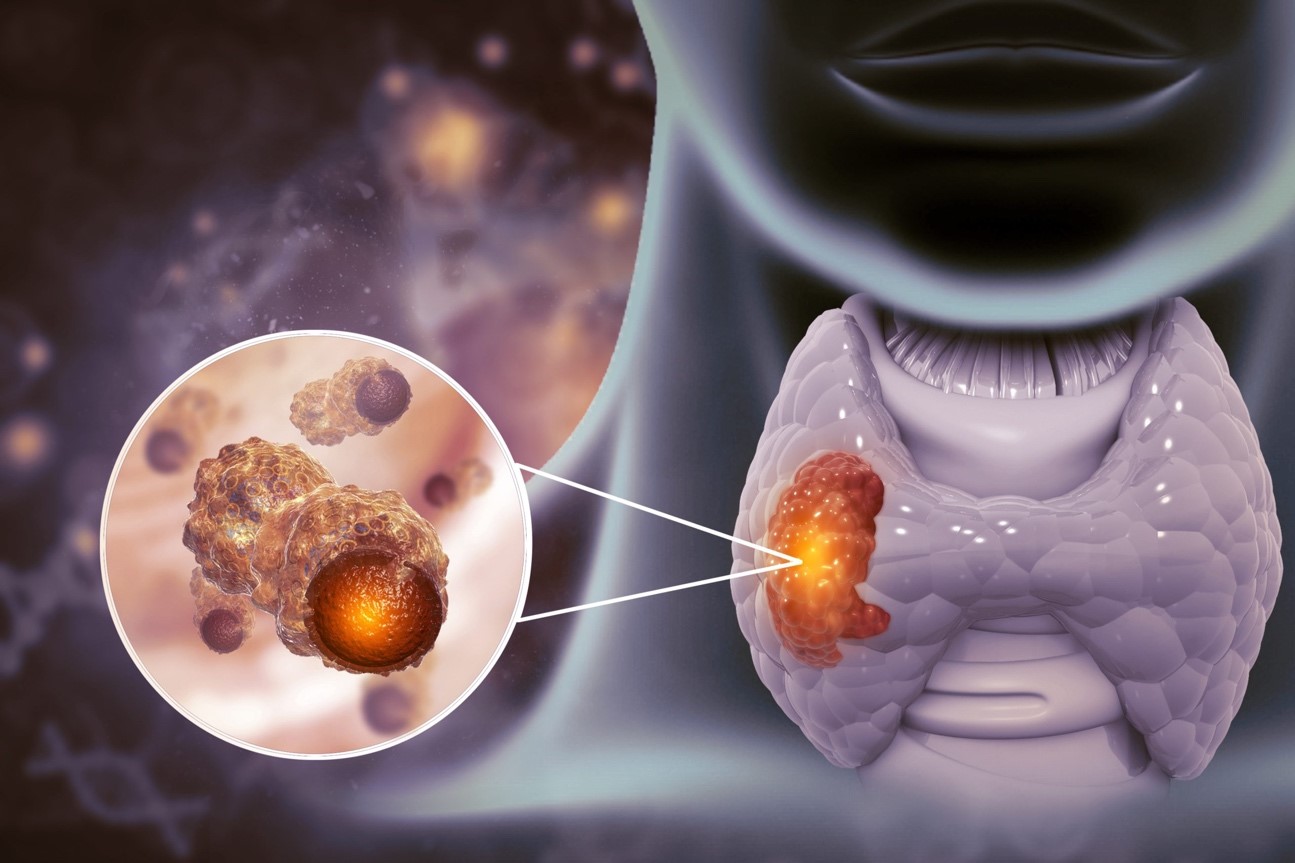
Cervical cancer is caused by at least 12 types of HPV – these are called oncogenic/high risk strains. These high-risk strains can also lead to cancers of the oropharynx, vagina, vulva, penis and anus, but these cancers are much rarer than cervical cancer. The rest of the HPV types may cause genital warts.
Cervical cancer is the 4th most common cancer among women globally and the 10th most common cancer among Singaporean women.
Myth #1: Only women who have sex often get HPV
Many people believe that women who have sex frequently have a higher risk of getting HPV. The number of sexual partners can increase the chance of exposure. However, the truth is that any women who has had sex, even with just one partner, could have been exposed to HPV.
It is believed that about 80% of women would have had HPV at some point in time by the age of 50.
Myth #2: A regular Pap test is enough to protect women against cervical cancer
The Pap test looks for abnormal cells on the cervix. The accuracy however is only 60%. That means that 40% of precancerous changes can be missed. Thankfully, the disease process of HPV infection to pre-cancerous changes and eventually cancer takes years. Regular repeating of the PAP smears will increase detection rate.
HPV is responsible for 99% of cervical cancer. The HPV test detects the DNA of high-risk DNA with high accuracy. Hence a negative result is very reassuring.
For women older than 30, getting the HPV test either along with, or in place of a Pap test increases the ability to identify women at risk to nearly 100%. Women under the age of 30 should get the HPV test if their Pap results are inconclusive.
Myth #3: If you have HPV, you will definitely get cervical cancer
Having HPV does not mean you have or will get cervical cancer. The infection usually goes away on its own, cleared by the immune system. Most people will not even know that they ever had HPV.
In about 10% of infections, the infection can persist over a longer period of time, causing abnormal cells to form which then develop into cervical cancer. The cervical cancer screening program aims to pick up these women for closer monitoring and treatment.
If the HPV infection causes pre-cancerous cell changes, these can be detected and treated early before cervical cancer has the chance to develop.
Myth #4: Women with HPV will experience symptoms
Most people with HPV do not know they are infected and never develop symptoms or health problems from it.
Although some low-risk types of HPV can cause genital warts – these do not become cancerous. The high-risk types that are associated with cervical cancer can cause changes in the form of abnormal cells which do not have symptoms and often go completely undetected until cancer develops
Hence, it is recommended to go for regular screening to identify the cancer in its early stages, increasing your chances of recovery.
Latest Articles
How Are Abdominal Hernias Treated?
What to Expect from Colorectal Surgery
How to Treat Breast Inflammatory Conditions
Gynaecomastia: Understanding Male Breast Cancer
Myth #5: The only way I can prevent cervical cancer is through Pap or HPV testing
Besides the HPV vaccination, your risk for cervical cancer can be minimized by avoiding the following:
- Smoking
- Multiple sexual partners
- Sexual intercourse at an early age
- STD infections such as Chlamydia infection
- Weakened immune system or HIV infection
Myth #6: If you get the HPV vaccination, you no longer need Pap or HPV testing
The HPV vaccine only protects against up to 9 of the 12 types of cancer-causing HPV types. Even then, vaccination is only fully effective when given to women who have not yet been exposed to HPV. The efficacy of the vaccine drops when given to women older than 27 and women who have been sexually active.
The ideal candidate for the vaccine is an adolescent girl or young women aged 9- 27 who has not been sexually active.
Regardless of the vaccination status, all women who are sexually active, should go for regular Pap and/or HPV testing.
Myth #7: An abnormal Pap test means cervical cancer
An abnormal Pap test usually picks up precancerous changes rather than cervical cancer. The abnormality can be caused by factors other than the presence of precancerous cells.
When a Pap test comes back as “abnormal”, there are different levels of grading of the abnormalities. This grading will assist your doctor in determining the possibility of pre cancer. The most common grading will be “atypical cells of unknown significance” – which can be caused by dryness, a local irritation, a non-HPV infection or a low-risk HPV type.
An abnormal PAP test will require assessment by a gynaecologist to determine the next step of intervention.
Myth #8: Cervical cancer is hereditary
Unlike breast cancer and ovarian cancer, cervical cancer is not hereditary. It is primarily caused by HPV infection.
The earlier cervical cancer is detected, the higher the chances of achieving a cure. Therefore, it is important that every sexually active woman follows cervical cancer screening recommendations.
Conclusion
With HPV testing, women with certain high-risk HPV infections can be identified and monitored carefully. Early detection of cervical cancer has been proven to significantly improve survival and quality of life.
If you are above the age of 30, you can visit a gynaecologist to get the HPV test along with a Pap test regardless of whether you have had a HPV vaccination. Meanwhile, women under the age of 30 should get the HPV test if their Pap results are inconclusive.
WHO WE ARE
About SOG Health Pte. Ltd.
Established in 2011, SOG Health Pte. Ltd. (“SOG”) is a leading healthcare service provider dedicated to delivering holistic health and wellness services to the modern family.
With a long and established track record in Singapore providing Obstetrics and Gynaecology (“O&G”) services such as pre-pregnancy counselling, delivery, pregnancy and post-delivery care, the Group has since further expanded its spectrum of healthcare services to include Paediatrics, Dermatology, and Cancer-related General Surgery (Colorectal, Breast & Thyroid).
The Group’s clinics, under its four operating segments of O&G, Paediatrics, Oncology and Dermatology, are strategically located throughout Singapore to provide easy access to its patients.
- Obstetrics
- Gynaecology
- GynaeOncology
- Breast, Thyroid & General Surgery
- Colorectal, Endoscopy & General Surgery
- Dermatology
- Paediatrics
Consult With A Specialist From SOG
Visit one of our specialists today to learn more about your health!
Recommended Specialists
Book An Appointment
Fill up this form and our clinic will get back to you shortly.
For general enquiries, please click here.